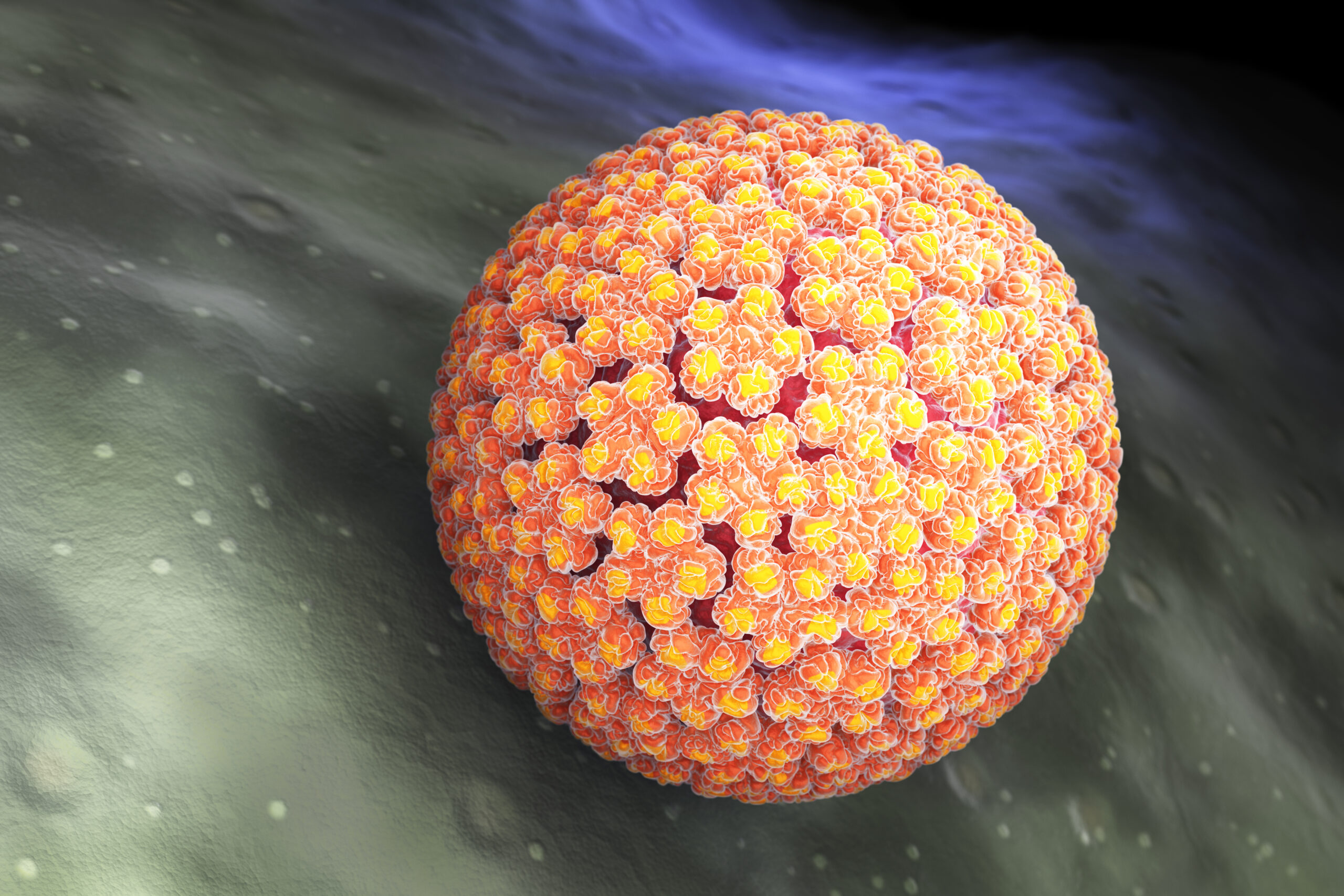
Most of us carry strains of human papillomavirus (HPV) on our skin without ever knowing it. Traditionally, these “skin-loving” viruses were thought to be harmless bystanders in the development of skin cancers. However, new research is challenging that assumption.
A recent case highlights how one of these HPV strains can directly contribute to tumor growth when the immune system is compromised. Cutaneous squamous cell carcinoma (cSCC), a cancer arising from the skin’s outer layer, is more common than often recognized, with millions of cases diagnosed in the U.S. each year.
HPV and Tumor Growth: A Surprising Connection
Researchers at the National Institutes of Health studied a 34-year-old woman with a recurring forehead tumor. They discovered that the tumor contained DNA from betapapillomavirus type 19 (beta-HPV), a virus normally considered harmless. Despite repeated surgeries and immunotherapy, her tumor persisted—until she received a stem cell transplant that restored her T-cell function. Following the transplant, the tumor stopped returning, illustrating how her immune system and the virus were intricately connected to the cancer’s behavior.
How the Virus Took Advantage
Beta-HPV usually lives on the skin without causing harm. In this patient, however, a rare genetic defect in ZAP70—a protein essential for T-cell activation—meant her immune system couldn’t properly respond to the virus. The viral genome integrated into the tumor’s DNA and produced viral proteins, effectively fueling tumor growth.
Laboratory tests confirmed that UV light damage alone wasn’t driving the cancer. Instead, it was the combination of the viral infection and the immune defect that created a perfect storm for cancer development.
Turning the Tide with Stem Cell Transplant
Doctors performed an allogeneic hematopoietic stem cell transplant, using donor cells to rebuild her immune system. This intervention restored T-cell function, cleared the virus, and stopped the tumor from recurring. The case underscores the importance of treating the underlying immune problem, not just the tumor itself, in select patients.
Implications for Patients and Clinicians
This discovery has potential implications for patients with aggressive cSCC, particularly those with immune deficiencies. Testing tumors for viral DNA may help identify cases where the virus is driving cancer growth, and strategies that support immune function could be key to long-term remission.
While this case involved a beta-HPV strain—not the alpha types targeted by current vaccines—it highlights the broader value of viral prevention. Vaccination programs have already significantly reduced rates of cervical precancer caused by alpha-HPV, demonstrating how stopping viral infections early can prevent cancers later.
Looking Ahead
Questions remain about how often beta-HPV drives cancer in immunocompromised patients and whether targeted antiviral or immune therapies could benefit them. Ongoing research will help determine which patients might gain from these approaches.
This case is a powerful reminder of the interplay between viruses, the immune system, and cancer—and the value of precision approaches in medicine.