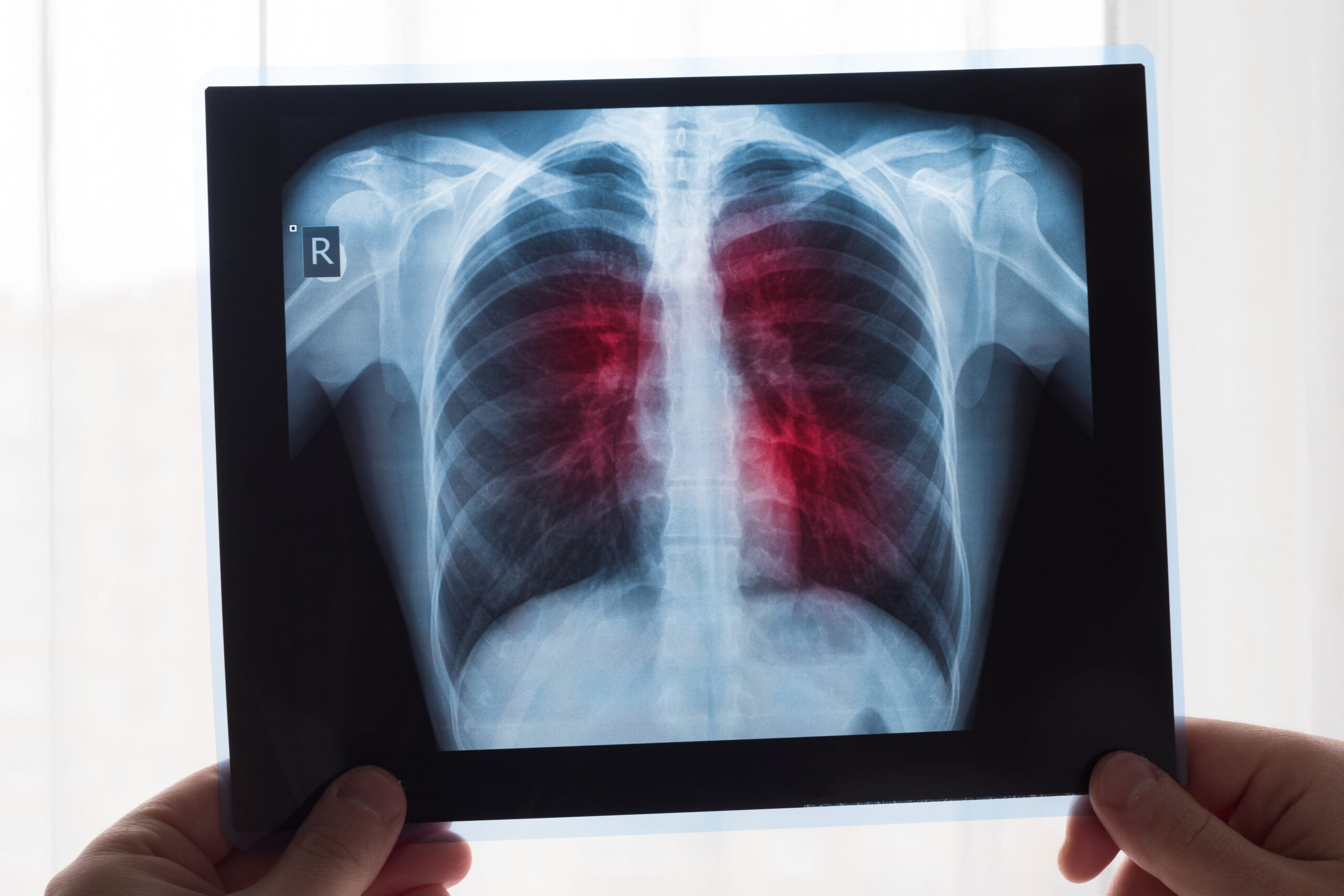
Catheter-Directed & Mechanical Thrombectomy Innovations
1. AlphaVac F18 Mechanical Aspiration System
- The APEX‑AV trial, evaluating a mechanical aspiration thrombectomy device (AlphaVac F18; AngioDynamics) in intermediate‑risk PE, showed meaningful reductions in right ventricle-to-left ventricle (RV/LV) ratio (~29%) and clot burden (~35.5%) at 48 hours, with acceptable safety profiles. This device received FDA 510(k) clearance for PE in April 2024.HealioThe Wall Street JournalMedscape
2. Hēlo PE (ENGULF Trial)
- The ENGULF trial tested a novel thrombectomy system featuring an expandable funnel and internal agitator for clot disruption. It achieved a 23.2% mean reduction in RV/LV ratio at 48 hours post-procedure, with no major adverse events or deaths at 30 days.HealioEurekAlert!SCAI
3. FlowTriever Device – FLASH & FLAME Studies
- FLASH registry and the FLAME study are evaluating the FlowTriever device in high- and intermediate-risk PE. Early findings show very low in-hospital mortality (~1.9%), compared to 29.5% in standard therapy cohorts.Lippincott Journals
Ultrasound-Enhanced Thrombolysis (USCDT)
- A robust real-world analysis (REAL‑PE) comparing ultrasound-assisted catheter-directed thrombolysis (USCDT) with mechanical thrombectomy (MT) found that USCDT had lower rates of major bleeding and hemoglobin reduction, although in-hospital mortality and length of stay were similar between the two.EurekAlert!
- Meta-analyses and studies suggest USCDT may better improve cardiopulmonary parameters and reduce bleeding risk compared to systemic thrombolysis.WikipediaEurekAlert!
Bashir Endovascular Catheter (BEC)
- The Bashir catheter (Thrombolex) uses an expandable basket design for enhanced drug delivery into clots. In the RESCUE trial:
- RV/LV ratio dropped by 33%
- Clot burden reduced by 35.9%
- Major bleeding rate was <1%
- Average hospital stay: 2.8 days
- This device received FDA clearance in April 2023.PMC
Emerging Mechanical Thrombectomy Techniques
Milli-Spinner Thrombectomy
- A novel approach involving a “milli‑spinner” technology that densifies fibrin networks mechanically and ejects red blood cells—resulting in up to 90% clot volume reduction in in-vitro and in-vivo models. This method targets clot structure rather than fragmenting it, potentially reducing distal embolism risk and improving efficacy.arXiv
Digital & AI-Enhanced Support
- Although not an intervention per se, new AI-driven models may advance patient management. For example, PEP‑Net, combining 3D ResNet and XGBoost, achieved ~94–94.5% accuracy in predicting 30-day in-hospital mortality based solely on initial CT scans.arXiv
- Additionally, large language models (LLMs) are being evaluated for automating extraction of PE-related data from radiology reports, offering potential to streamline registry data handling.arXiv
Summary Table
| Innovation | Highlights |
| AlphaVac F18 | FDA-cleared mechanical aspiration, 29% RV/LV reduction |
| Hēlo PE (ENGULF) | Expandable funnel device, safe with 23% RV/LV improvement |
| FlowTriever (FLASH/FLAME) | Very low mortality (~1.9%) in high-risk PE |
| USCDT (Ultrasound-assisted) | Fewer bleeding complications, effective thrombolysis |
| Bashir Catheter (BEC) | Basket delivery with low bleeding, short hospital stay |
| Milli‑spinner Thrombectomy | High-volume clot reduction via microstructural disruption |
| AI Tools (PEP‑Net, LLMs) | Enhanced prognosis prediction and data abstraction automation |
Bottom Line
There’s a noticeable shift toward minimally invasive, catheter-based mechanical and pharmacomechanical strategies for PE that offer improved efficacy, safety, and quicker recovery. Devices like AlphaVac, Hēlo, FlowTriever, Bashir BEC, and the emerging milli-spinner show particular promise. Ultrasound-assisted thrombolysis continues to hold therapeutic appeal due to lower bleeding risks. Meanwhile, AI tools are emerging to support decision-making and institutional data handling.